So many readers have asked me to comment on the American Academy of Pediatrics’ Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity that I thought I ought to say something about it.
The guideline report is so long and detailed that I cannot imagine anyone actually reading it.
I started with the introduction, which summarizes basic facts.- 14.4 million children and adolescents are affected by obesity.
- Obesity is a chronic disease with potentially serious health consequences
- Childhood obesity is strongly affected by social determinants of health (poor education, poverty, racism, exposure to toxins, etc)
- Childhood obesity is stigmatized in ways that fail to acknowledge social determinants.
What got press attention—and the attention of readers of this blog—is the AAP’s endorsement of drug and bariatric surgical treatment of obese children.
I cut right to the chase and looked at Appendix I, which gives the AAP’s algorithm for deciding on treatment options.

The report’s major conclusions expand on this chart (the report does not define KAS, but I think it means Knowledge, Attitudes, and Skills):
KAS 9. Pediatricians and other PHCPs should treat overweight (BMI ≥ 85th percentile to <95th percentile) and obesity (BMI ≥ 95th percentile) in children and adolescents, following the principles of the medical home and the chronic care model, using a family-centered and nonstigmatizing approach that acknowledges obesity’s biologic, social, and structural drivers.
KAS 10. Pediatricians and other PHCPs should use motivational interviewing (MI) to engage patients and families in treating overweight (BMI ≥ 85th percentile to <95th percentile) and obesity (BMI ≥ 95th percentile).
KAS 11. Pediatricians and other PHCPs should provide or refer children 6 y and older (Grade B) and may provide or refer children 2 through 5 y of age (Grade C) with overweight (BMI ≥ 85th percentile to <95th percentile) and obesity (BMI ≥ 95th percentile) to intensive health behavior and lifestyle treatment. Health behavior and lifestyle treatment is more effective with greater contact hours; the most effective treatment includes 26 or more hours of face-to-face, family-based, multicomponent treatment over a 3- to 12-mo period.
KAS 12. Pediatricians and other PHCPs should offer adolescents 12 y and older with obesity (BMI ≥ 95th percentile) weight loss pharmacotherapy, according to medication indications, risks, and benefits, as an adjunct to health behavior and lifestyle treatment.
KAS 13. Pediatricians and other PHCPs should offer referral for adolescents 13 y and older with severe obesity (BMI ≥ 120% of the 95th percentile for age and sex) for evaluation for metabolic and bariatric surgery to local or regional comprehensive multidisciplinary pediatric metabolic and bariatric surgery centers.
What is not in this guideline is anything that addresses the social determinants of childhood obesity. What we have here is a focus on treating the symptoms, but getting nowhere near the cause.
It is difficult for someone like me who is not affected by those determinants to even imagine how drugs and surgery could be thought even remotely acceptable for children, even those over the age of 12, but I am not treating these kids.
Providers who do treat obese children tell me they are relieved to be able to offer options that might help kids achieve healthier weights.
As I see it, these should be absolute last resorts if used at all. And this is without even getting into issues of cost or our dysfunctional health care system.
In public health terms, drugs and surgery are “downstream” solutions to a problem that began way upstream with all those societal determinants.
If ever we needed upstream approaches, chldhood obesity is a prime example.
Upstream means policy changes that make healthy eating more appealing, accessible, and affordable That’s what pediatricians need to be calling for.
This AAP report deliberately separates treatment from prevention. It promises a discussion of prevention in a subsequent report. I hope it is as hard hitting as any AAP report has ever been.
If childhood obesity teaches us anything, it is that our society needs to change in ways that are healthier for our children.
Additional supporting documents
- Executive Summary: Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity
- Appraisal of Clinical Care Practices for Child Obesity Treatment. Part I: Interventions
- Appraisal of Clinical Care Practices for Child Obesity Treatment. Part II: Comorbidities
Thanks to all the people who wrote me about this. Much appreciated.
*******
For 30% off, go to www.ucpress.edu/9780520384156. Use code 21W2240 at checkout.
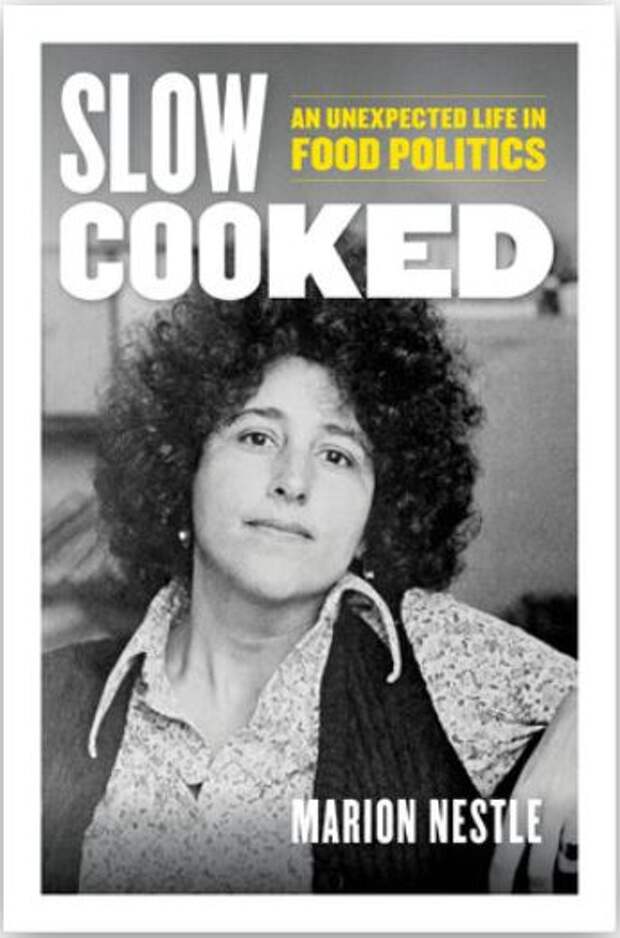
The post Do we need drugs and surgery to treat childhood obesity? Surely there are better ways. appeared first on Food Politics by Marion Nestle.